Dry socket (also known as alveolar osteitis) is one of the most commonly presenting complications after extraction of impacted third molars (i.e. wisdom teeth), occurring in 25-30% of impacted wisdom tooth extractions, and 0.5-5% of routine dental extractions. Dry socket usually occurs when the blood clot (i.e. thrombus) does not form or is lost, resulting in an empty socket where bone is exposed to the oral cavity. The subsequent localized alveolar osteitis is limited to the bone that lines the socket (the lamina dura).
Pyrexia and cervical lymphadenitis are not typically present in dry socket cases as it is not primarily an infection, there is typically also only minimal edema and erythema present in soft tissues surrounding the socket. Patients usually experience a dull, aching, throbbing pain around the socket two-four days after extraction. This pain may radiate peripherally to the ear, eye, temple, and neck, and may vary in severity from moderate to severe. Patients may also experience intraoral halitosis, or a bad taste in their mouth.
While the direct cause of dry socket is unknown, a number of factors that increase one’s likelihood of experiencing a dry socket have been identified. Conditions that could result in hypovascularity of the alveolar bone such as Paget’s disease and cemento-osseous, however some have made an effort to distinguish this from “true alveolar osteitis”. Other factors shown to increase risk for developing a post-operative dry socket are:
Pre-existing infection
Smoking
Surgical Trauma
Usage of vasoconstrictors
Radiotherapy directed at the bones of the jaw
Hormonal changes caused by the menstrual cycle while taking oral contraceptives
Lastly, the site in which the tooth was extracted can be considered in the likelihood to develop a dry socket, as they more commonly occur in the mandible as opposed to the maxilla. The mandible has a comparatively poorer blood supply than the maxilla, and food debris will tend to gather more readily in lower sockets than upper ones.
Treatment is normally directed at reducing the patients’ pain as well as addressing any other symptoms. Irrigation with saline or local anesthetic to remove and debris from the socket is commonly necessary as well. Medicated dressings, typically antibacterials, anesthetics, and/or obtundants are also commonly used, however they act as a foreign body which prevents healing. Consequently, they are normally only used until pain has been reduced.
Chlorhexidine, which is a bisdiguanide antiseptic with antimicrobial properties has shown to lower the rate at which patients develop a dry socket when used to rinse with. Literature has been somewhat split on the use of antibiotics to prevent dry socket, as it has shown to be beneficial in the prevention of dry socket, however has mild adverse effects. Lastly, prevention of dry socket has been shown to increase by following post-operative instructions.
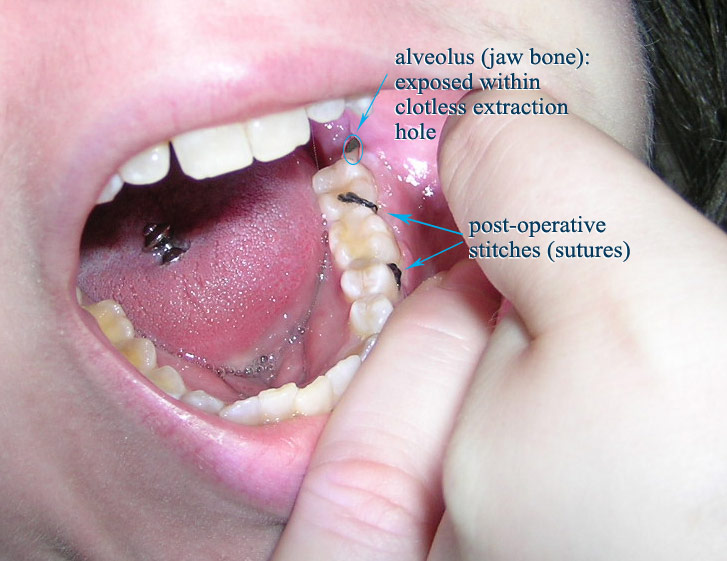
A dry socket. (Beatgoddess [CC BY 3.0 (https://creativecommons.org/licenses/by/3.0)])